|
# # # # Lysosomes are small bags of enzymes that are used to break down material inside of cells – digesting newly absorbed food or recycling old/used proteins and rubbish. Recently researchers have been discovering increasing evidence that points towards dysfunction in lysosomes as a key influential player in neurodegenerative conditions, like Parkinson’s. There are several Parkinson’s genetic risk factors associated with lysosomal function (GBA being the obvious one), that can increase one’s risk of developing Parkinson’s. But there is also data indicating that individuals without any of these risk factors may also have reduced lysosomal activity. And recently researchers have identified one possible explanation. In today’s post, we will explore what lysosomes are, investigate how they maybe involved with Parkinson’s, review what the new data reports, and discuss how this information might be useful. # # # # |
 Type of endocytosis. Source: Slidemodel
Type of endocytosis. Source: Slidemodel
On a continual basis, cells inside your body are absorbing material from the world around them with the aim of collecting all that they need to survive. They do this predominantly via a process called endocytosis, in which a small part of the cell membrane envelopes around an object (or objects) and it is brought inside the cell.
As the section of cell membrane enters the interior of the cell, it detaches from the membranes and forms what is called an endosomes (sometimes it is also called a vacuole). Once inside, the endosome transported deeper into the interior of the cells where it will bind to another small bag that is full of digestive enzymes that help to break down the contents of the endosome.
This second bag is called a lysosome.

How lysosomes work. Source: Prezi
Once bound, the lysosome and the endosome/vacuole will fuse together and the enzymes from the lysosome will be unleashed on the material contained in the vacuole. The digestion that follows will break down the material into more manageable components that the cell needs to function and survive.
This enzymatic process works in a very similar fashion to the commercial products that you use for washing your clothes.
 Enzymatic degradation. Source: Samvirke
Enzymatic degradation. Source: Samvirke
The reagents that you put into the washing machine with your clothes contain a multitude of enzymes, each of which help to break down the dirty, bacteria, flakes of skin, etc that cling to your clothes. Each enzyme breaks down a particular protein, fat or such like. And this situation is very similar to the collection of enzymes in the lysosome. Each enzyme has a particular task and all of them are needed to break down the contents of the endosome.
Interesting, but what does this have to do with Parkinson’s?
Well, increasingly it is becoming apparent that lysosomes may be playing a role in underlying biology of Parkinson’s.
This statement is largely based on the observation that a number of the genetic risk factors that increase the risk of developing Parkinson’s are associated with proteins involved in lysosomal function.
In fact, a report published in 2017 found that the many people with Parkinson’s also have a genetic risk factor for other lysosome-related conditions.
This is the report here:
Title: Excessive burden of lysosomal storage disorder gene variants in Parkinson’s disease.
Authors: Robak LA, Jansen IE, van Rooij J, Uitterlinden AG, Kraaij R, Jankovic J; International Parkinson’s Disease Genomics Consortium (IPDGC), Heutink P, Shulman JM; IPDGC Consortium members; International Parkinson’s Disease Genomics Consortium (IPDGC).
Journal: Brain. 2017, 140(12): 3191–3203.
PMID: 29140481 (This report is OPEN ACCESS if you would like to read it)
In this study, the researchers focused their analysis on genetic risk factors associated with 54 different lysosomal disorder. They screened the DNA collected from 1156 individuals with Parkinson’s and 1679 unaffected “control” participants.
The investigators found that over half (56%) of the Parkinson’s cases they analysed had at least one genetic risk factor for a lysosomal condition (and 21% had more than one). And this result was consistent across two independent cohorts (cohort 1. containing 436 PD cases and 169 controls, and cohort 2. containing an additional 6713 PD cases and 5964 controls).
The researchers concluded that multiple genetic hits may act in combination to degrade overall lysosomal function, which in turn could enhance Parkinson’s susceptibility (perhaps by reducing the clearance of waste proteins in cells).
Lysosomes are involved with clearance of cellular waste?
In addition to breaking down material in endosomes, lysosomes are also involved waste disposal. They help to break down and recycle (or dispose of) old/used proteins in a process called autophagy.
What is autophagy?
Autophagy (from the Ancient Greek αὐτόφαγος autóphagos, meaning “self-devouring”) is an absolutely essential function in a cell. Without autophagy, old proteins would pile up, making the cell sick and eventually causing it to die. Through the process of autophagy, the cell can break down the old protein, clearing the way for fresh new proteins to do their job.

The process of autophagy. Source: Wormbook
Waste material inside a cell is collected in membranes that form sacs (called autophagosomes), which then bind to lysosomes. As the two fuse, the enzymes inside the lysosome breakdown and degrade the waste material. The degraded waste material can then be recycled and used again, or be disposed of – by spitting it out of the cell (the reverse process of endocytosis – called exocytosis).
|
# RECAP #1: Lysosomes are small sacs inside of cells that contain enzymes that are used to breakdown material that has been imported into the cell (via a process called endocytosis) or to breakdown old proteins that need to be disposed of (a mechanism called autophagy). Properly functioning lysosomes are a critical aspect of normal cellular life. # |
Can you give an example of a Parkinson’s associated protein that is involved with lysosomal function?
Sure.
The best example of a Parkinson’s-associated protein involved in lysosomal function is glucocerebrosidase (also known as GCase).
What does GCase do?
Glucocerebrosidase (or GCase) functions as one of the enzymes inside lysosomes. It helps with the digestion and recycling of proteins (particularly glucocerebrosides) inside lysosomes.
The instructions for making GCase are provided by a region of DNA (a gene) called GBA.
Ok, but how is GCase associated with Parkinson’s?
Many years ago, it was discovered that tiny genetic variations in the GBA gene are associated with a condition called Gaucher disease.
Gaucher (pronounced “go-shay”) disease is a rare inherited lysosomal storage disorder. It is characterised by the build up in lysosomes of the lipid glucocerebroside. Because the body cannot break it down, swollen cells start to build up in certain areas of the body, such as the spleen, liver and bone marrow. These cells are referred to as ‘Gaucher cells’.
 Swollen Gaucher cells (circled in red). Source: Imagebank
Swollen Gaucher cells (circled in red). Source: Imagebank
But in the 1990s, physicians began to notice that patients with Gaucher disease appeared to have a higher risk of developing Parkinson’s. An example of this was a report published in 1996 that described individuals with Gaucher disease who also exhibited an early-onset, severe form of Parkinson’s with a stronger element of cognitive decline:
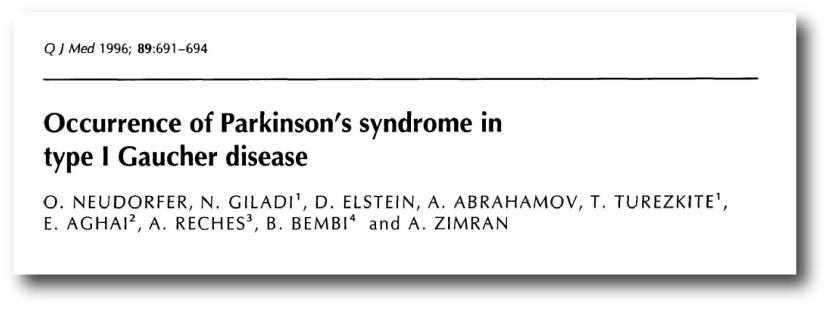 Title: Occurrence of Parkinson’s syndrome in type I Gaucher disease.
Title: Occurrence of Parkinson’s syndrome in type I Gaucher disease.
Authors: Neudorfer O, Giladi N, Elstein D, Abrahamov A, Turezkite T, Aghai E, Reches A, Bembi B, Zimran A.
Journal: QJM. 1996 Sep;89(9):691-4.
PMID: 8917744 (This article is OPEN ACCESS if you would like to read it)
In this study, the Israeli researchers reported on 6 people with Type I Gaucher disease (which up until that point had not been considered neuronopathic). All six of the subjects also exhibited the hallmarks of a rather severe form of Parkinson’s, which made its appearance in the 4th to 6th decade of life and displayed an aggressive progression and was largely unresponsive to conventional anti-Parkinson therapy (such as L-dopa).
Larger follow up studies have reported similar situations (Click here and here for an example).
So people with Gaucher disease have a higher risk of developing Parkinson’s?
Yes, but there is more.
There are a lot of people who do not have Gaucher disease, but do have a genetic variant in their GBA gene. And since the early Gaucher-Parkinson’s studies were published, we have gone on to discover that a sizable portion of the Parkinson’s affected community have GBA variations.
In fact, GBA variants are some of the most common genetic risk factors for Parkinson’s. It is believed that approximately 5%–8% of people with Parkinson’s may have a genetic mutation in their GBA gene (Click here and here to read more about this).
How does GBA variants result in increased risk of Parkinson’s?
This is not yet thoroughly understood, and it may differ depending on the type of genetic variation.
In general, in healthy unaffected individuals, the enzyme glucocerebrosidase (or GCase) helps to break down proteins and helps to maintain proper lysosomal function (lysosomes are small bags inside of cells where the enzyme conducts its job).
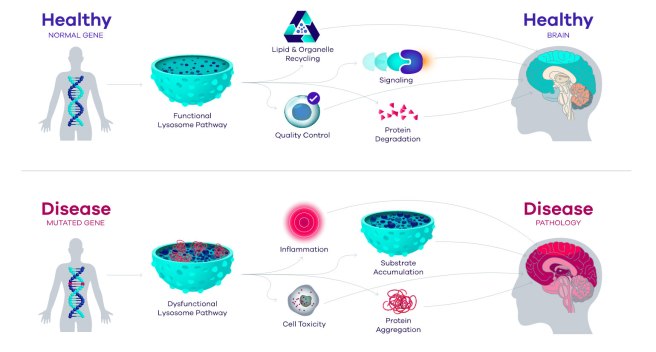 Source: Prevail
Source: Prevail
In individuals with GBA genetic variations, however, it is believed that the enzymatic breakdown of proteins is disrupted, which results in the build up and accumulation of proteins. This can lead to inflammation and ultimately cell death. And this process is believed to give rise to the appearance of Parkinson’s symptoms.
But this GBA/lysosomal function issue only affects people with GBA variants?
Well, actually…
There are now numerous reports that GCase activity is reduced in people with idiopathic Parkinson’s – that is, people with spontaneous Parkinson’s that can not be attributed to a particular genetic variant (Click here to read an example of this research).
There are also reports that GCase activity in the brain reduces as all of us get older:
 Title: Progressive decline of glucocerebrosidase in aging and Parkinson’s disease.
Title: Progressive decline of glucocerebrosidase in aging and Parkinson’s disease.
Authors: Rocha EM, Smith GA, Park E, Cao H, Brown E, Hallett P, Isacson O.
Journal: Ann Clin Transl Neurol. 2015 Apr;2(4):433-8.
PMID: 25909088 (This report is OPEN ACCESS if you would like to read it)
In this study, the researchers collected frozen postmortem brain tissue from both male and female sporadic Parkinson’s patients and neurologically unaffected control cases. They then measured GCase activity in substantia nigra and putamen – two regions of the brain that are severely affected by Parkinson’s.
The investigators found that GCase activity in control (non-Parkinson’s) cases decreased in the substantia nigra and the putamen across the sixth to eighth decades of life – indicating an age-associated decline in GCase activity.
Source: PMC
But importantly, this reduction in GCase activity was lower in idiopathic Parkinson’s cases across many of these decades of life (in both the putamen and substantia nigra).
 Source: PMC
Source: PMC
And remember that these Parkinson’s cases did not have any genetic variations in their GBA genes.
So something strange is occurring as we age that results in lower levels of GCase activity in everyone, but this effect is exacerbated for some reason in some people with Parkinson’s (without GBA variants).
Recently the researchers who published the study described above, have presented new data that could point towards one possible explanation.
Here is their report:
 Title: Fibroblasts from idiopathic Parkinson’s disease exhibit deficiency of lysosomal glucocerebrosidase activity associated with reduced levels of the trafficking receptor LIMP2.
Title: Fibroblasts from idiopathic Parkinson’s disease exhibit deficiency of lysosomal glucocerebrosidase activity associated with reduced levels of the trafficking receptor LIMP2.
Authors: Thomas R, Moloney EB, Macbain ZK, Hallett PJ, Isacson O.
Journal: Mol Brain. 2021 Jan 19;14(1):16.
PMID: 33468204 (This report is OPEN ACCESS if you would like to read it)
To better understand why reductions in GCase activity were occurring in people with idiopathic Parkinson’s, the researchers collected skin cells (called fibroblasts) from 31 cases of idiopathic Parkinson’s, 6 people with GBA-associated Parkinson’s (N370S variant), and 15 control volunteers. They grew the cells in culture and analysed them all for GCase activity.
The investigators found that the cells from people with idiopathic Parkinson’s (no mutations in the GBA gene) exhibited reduction in lysosomal GCase activity that were similar to that observed in the cells from people with GBA-associated Parkinson’s. As you can see in the image below, in graph A, the GCase activity in the idiopathic Parkinson’s cases (red bar) were reduced compared to the control cases (white bar), and in many cases similar to the GBA-associated PD cases (grey bar).
 Source: PMC
Source: PMC
The researchers analysed levels of GBA mRNA in all of the cells – mRNA is the instructions for making proteins – but they found no difference between the three groups (panel B in the image above). So, something odd is happening to GCase during protein production or on the journey to the lysosome.
Scratching their heads, the researchers then shifted their attention to proteins that are involved with transporting GCase from the endoplasmic reticulum to the lysosome.
What is the endoplasmic reticulum?
The endoplasmic reticulum (or ER) is a highly convoluted, net-like mesh structure that extends off the nucleus. It is the assembly line where proteins are produced within a cell.
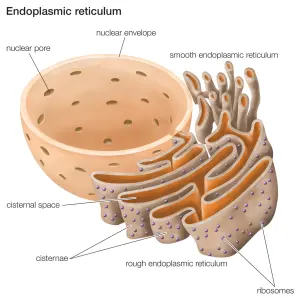 The endoplasmic reticulum. Source: Britannica
The endoplasmic reticulum. Source: Britannica
The nucleus is where the blue prints for making and maintaining an organism is kept in the form of DNA. As mentioned above, a template of how to produce a particular protein can be generated from this DNA and that template is called mRNA.
mRNA is used to produce a protein (via a process called translation). A large part of that protein production process is conducted within the endoplasmic reticulum.
When GCase enzyme is produced in the ER, it is transported to lysosomes by a protein called Lysosomal integral membrane protein 2 (or LIMP2).
 Source: NIH
Source: NIH
LIMP2 binds to GCase in the ER and transports it all the way to the lysosome, where is releases it and the GCase can then do its job.
Genetically engineered mice with no LIMP2 exhibit significantly reduced levels of GCase activity and in some areas of the brain there are increased levels of the Parkinson’s-associated protein alpha synuclein in combination with lysosomal dysfunction (Click here to read more about this).
So LIMP2 is obviously important for GCase function in cells.
When the researchers looked at LIMP2 in their skin cells growing in culture, they found that the reduced GCase enzyme activity in the idiopathic Parkinson’s cells was accompanied by a similar reduction in both LIMP2 mRNA and protein:
 Source: PMC
Source: PMC
And this reduction in LIMP2 resulted in a build up of GCase protein in the ER of these cells:
 Source: PMC
Source: PMC
These findings pointed towards LIMP2 possibly being responsible for the reduced GCase levels in some cases of idiopathic Parkinson’s.
The researchers concluded their study by stating “idiopathic Parkinson’s fibroblasts have decreased GCase activity primarily driven by altered LIMP2-mediated transport of GBA to lysosome“, and they suggested that the reduced levels of GCase activity observed in the GBA-associated Parkinson’s cells “occurs through a different mechanism“.
They also suggested that therapeutic treatments aimed at increasing the activity of lysosomal enzymes or increasing lysosomal enzyme transport through LIMP2 could serve as attractive future therapeutic targets.
|
# RECAP #2: Researchers report that the activity of the lysosomal enzyme GCase is reduced in the brain with normal aging. This reduction appears to be exaggerated in some people with Parkinson’s. New studies have identified a protein called LIMP2 as being potentially influential in this reduction of GCase activity. LIMP2 is required to transport GCase to the lysosome, where it can do its job. # |
Interesting. Has anyone ever seen this before?
Previous research has investigated LIMP2 and pointed towards an influential role in regulating GCase activity:
 Title: LIMP-2 expression is critical for β-glucocerebrosidase activity and α-synuclein clearance.
Title: LIMP-2 expression is critical for β-glucocerebrosidase activity and α-synuclein clearance.
Authors: Rothaug M, Zunke F, Mazzulli JR, Schweizer M, Altmeppen H, Lüllmann-Rauch R, Kallemeijn WW, Gaspar P, Aerts JM, Glatzel M, Saftig P, Krainc D, Schwake M, Blanz J.
Journal: Proc Natl Acad Sci U S A. 2014 Oct 28;111(43):15573-8.
PMID: 25316793 (This report is OPEN ACCESS if you would like to read it)
In this study, the investigators reported that loss of LIMP-2 in mice reduced the lysosomal activity of GCase, which resulted in a disruption to lysosomal function and an accumulation of Parkinson’s-associated α-synuclein. They also observed the loss of dopamine neurons and increased inflammation in the mice.
The research next explored the opposite scenario: what happens when you enhance LIMP2 levels?
They increased LIMP2 levels in cells in culture that already produced high levels of alpha synuclein, and they found that higher LIMP2 levels enhanced the lysosomal clearance of alpha synuclein protein, making the cells appear healthier.
Curiously, in this study, when the researchers looked at LIMP2 protein in the postmortem human brain, they observed increased levels of LIMP-2 in the surviving dopamine neurons of people who passed away with Parkinson’s. This finding conflicts with the skin cell findings above (and with a third study of the PD brain which reported no difference in LIMP2 levels in PD – click here to read that report).
The researchers suggest that the observed increase of LIMP2 in surviving dopamine neurons could be a “protective mechanism” – an attempt by the cells to boost lysosomal GCase activity to counter the effect of Parkinson’s. They point toward research showing similar data for other Parkinson’s-associated lysosomal proteins (such as ATP13A2/Park9 – click here to read more about that).
If LIMP2 needs to be boosted, how could that potentially be achieved?
So this is where the story gets interesting.
Several years ago, it was reported that the respiratory medication ambroxol could increase levels of LIMP2 in cells.
This is the report here:
 Title: Effects of ambroxol on the autophagy-lysosome pathway and mitochondria in primary cortical neurons.
Title: Effects of ambroxol on the autophagy-lysosome pathway and mitochondria in primary cortical neurons.
Authors: Magalhaes J, Gegg ME, Migdalska-Richards A, Schapira AH.
Journal: Sci Rep. 2018 Jan 23;8(1):1385.
PMID: 29362387 (This report is OPEN ACCESS if you would like to read it)
In this study, the researchers reported that when they treated mouse neurons with ambroxol, they saw an increase in levels of LIMP2 protein at the higher dose used:
 Source: PMC
Source: PMC
And this finding is supported by a previous study that reported ambroxol treatment increased LIMP2 protein levels in skin cells (fibroblasts) from people with GBA-associated Parkinson’s (Click here to read more about that report).
Ambroxol is currently of interest in the Parkinson’s research community as last year the result of a Phase II clinical trial of ambroxol demonstrated that the drug was safe and well tolerated in people with Parkinson’s.
Here is the report of the study:
 Title: Ambroxol for the Treatment of Patients With Parkinson Disease With and Without Glucocerebrosidase Gene Mutations: A Nonrandomized, Noncontrolled Trial.
Title: Ambroxol for the Treatment of Patients With Parkinson Disease With and Without Glucocerebrosidase Gene Mutations: A Nonrandomized, Noncontrolled Trial.
Authors: Mullin S, Smith L, Lee K, D’Souza G, Woodgate P, Elflein J, Hällqvist J, Toffoli M, Streeter A, Hosking J, Heywood WE, Khengar R, Campbell P, Hehir J, Cable S, Mills K, Zetterberg H, Limousin P, Libri V, Foltynie T, Schapira AHV.
Journal: JAMA Neurol. 2020 Jan 13. [Epub ahead of print]
PMID: 31930374 (This report is OPEN ACCESS if you would like to read it)
In addition, the researchers reported that the drug was entering the brain, and they recorded a 35% increase in GCase protein levels in the cerebrospinal fluid – this is the liquid surrounding the brain (Click here to read a previous SoPD post about that trial).
This clinical trial was supported by Cure Parkinson’s, the Van Andel Institute and the John Black Charitable Foundation, and they are now working with the researchers involved to continue the clinical development of ambroxol for Parkinson’s with a larger and longer study.
So what does it all mean?
Lysosomal function represents a major area of research in the Parkinson’s field. A number of genetic variations identified in some of the Parkinson’s-affected community point towards a disruption in the enzymatic break-down of cellular material as being associated with an increased risk of developing the condition.
Even in people unaffected by lysosome-associated genetic mutations, however, there is evidence that lysosomal activity is reduced with age, and this appears to be exaggerated in people with Parkinson’s (even in the absence of a lysosome-associated genetic variant).
Numerous clinical trial programmes are now ongoing with a focus on improving lysosomal function (ambroxol was discussed above, but biotech companies like Bial biotech, Prevail Therapeutics, and E-scape Bio are actively exploring this area). And novel lysosomal approaches are also being investigated – see upcoming SoPD post on TMEM175). It will be particularly interesting to see how these experimental therapies affect the different types of Parkinson’s (idiopathic PD, GBA-associated PD, etc).
 All of the material on this website is licensed under a
All of the material on this website is licensed under a
Creative Commons Attribution 4.0 International License
You can do whatever you like with it!
EDITOR’S NOTE: The author of this post is an employee of Cure Parkinson’s, so he might be a little biased in his views on research and clinical trials supported by the trust. That said, the trust has not requested the production of this post, and the author is sharing it simply because it may be of interest to the Parkinson’s community.
The information provided by the SoPD website is for information and educational purposes only. Under no circumstances should it ever be considered medical or actionable advice. It is provided by research scientists, not medical practitioners. Any actions taken – based on what has been read on the website – are the sole responsibility of the reader. Any actions being contemplated by readers should firstly be discussed with a qualified healthcare professional who is aware of your medical history. While some of the information discussed in this post may cause concern, please speak with your medical physician before attempting any change in an existing treatment regime.
The banner for today’s post was sourced from Youtube.



