Stem cell (dopamine cell replacement) therapies for Parkinson’s
Our recent Research Update meeting in February 2023 highlighted the recent updates in the field of cell replacement therapies for Parkinson’s with Professor Roger Barker. Watch this recording now:
In addition to the TRANSEURO study, there are a number of stem cell-based clinical trials of cell transplantation getting underway around the world. Professors Roger Barker, Malin Parmar, Claire Henchcliffe and Jun Takahashi are part of an international consortium of labs working on cell transplantation in Parkinson’s under the name of GForce-PD, Cure Parkinson’s hosted the sixth G-Force PD meeting in Cambridge in April 2019. Each lab in the GForce-PD group aims to bring dopamine replacement cell replacement therapy for Parkinson’s to clinical trial within the next few years.
There are two types of cells which are currently being developed for clinical testing in dopamine replacement cell transplantation for Parkinson’s. Embryonic stem cells (or ESCs) – which are collected from IVF tissue donation – and induced pluripotent stem cells (or iPSCs) – chemically reprogrammed cells, usually from adult skin tissue and blood cells. Both types of cells are capable of becoming almost any cell in the body, and scientists have been working on recipes for turning them into dopamine-producing cells. These significant trials are underway.
Induced Pluripotent Stem Cells
Transplantation is not the only application for iPSC cells. Scientists are making iPSC’s from patients with Parkinson’s and using them in the lab for disease modelling purposes. These neurons act as a powerful tool to study the neuropathology of Parkinson’s and they can be used to test substances developed into new drugs to effectively treat the condition.
The MRC Centre for Regenerative Medicine, University of Edinburgh
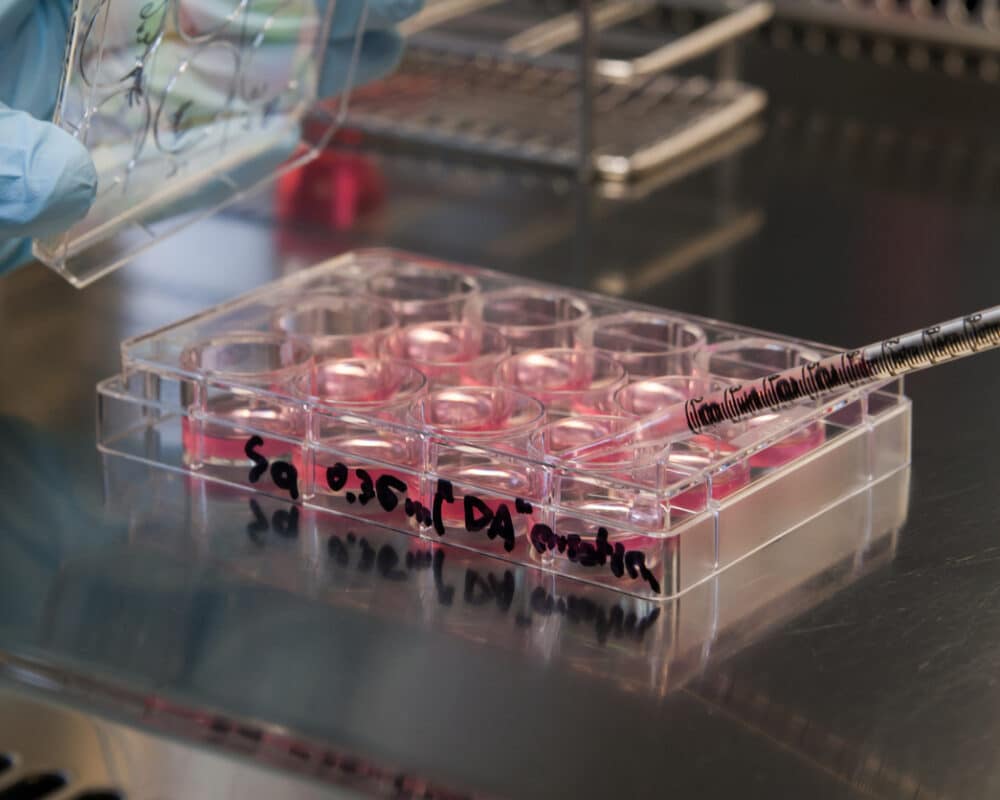
Prof. Tilo Kunath’s laboratory in Edinburgh is leading the way here and Cure Parkinson’s is providing funding for this research. Prof. Kunath is producing pure batches of dopamine neurons under a highly technical process that only a few laboraties in the world are capable of doing safely and effectively to better differentiate and characterise the cell lines which are planned to be used for transplantation.
Cure Parkinson’s is also funding a study led by Prof. Roger Barker, which involves converting a person with Parkinson’s own skin cells directly into neurons. These cells are called induced neuronal cells (or iN cells). The goal of the study is to provide a rapid method of growing patient-specific cells, which would allow for a more personalised form of testing potential Parkinson’s therapies in the laboratory.
Important news updates
July 2023
BlueRock Therapeutics reports positive results from its phase 1 clinical trial
February 2023
The California Institute for Regenerative Medicine (or CIRM) is a major funder of research focused on stem cell treatments and has agreed to provide $4 million to Ryne Bio to help bring their dopamine producing cell replacement therapy into the clinic for Parkinson’s.
November 2022
The STEM-PD study is highlighted in an article in the Guardian newspaper
May 2022
BlueRock Therapeutics announced that they have completed enrollment for their Phase 1 cell transplantation clinical trial in Parkinson’s
April 2022
Aspen Neuroscience launched their first patient screening study for their planned clinical trial of personalized cell transplantation in Parkinson’s.
January 2022
The Michael J Fox Foundation awarded grants to the ASU-Banner Neurodegenerative Disease Research Center for a clinical trial testing transplantion of human iPSC derived dopamine neurons into the brains of people with a special type of Parkinson’s due to Parkin mutations. This project will be in collaboration with the van Andel institute and Fujifilm Cellular Dynamics.
October 2021
The first Phase 1/2 clinical trial of a stem cell-based therapy in people with Parkinson’s has been approved by the Swedish Medical Products Agency.
June 2021
BlueRock Therapeutics Announces First Patient Dosed with DA01 in Phase 1 Study in Patients with Advanced Parkinson’s Disease
February 2021
Biotech company BlueRock Therapeutics received approval from the US Food and Drug Administration (FDA) to begin cell transplantation clinical trials in people with Parkinson’s.
January 2020
Prof. Malin Parmar and Prof. Claire Henchcliffe’s article: ‘The future of stem cell therapies for Parkinson disease’ is published in Nature Reviews Neuroscience on the current landscape of clinical trials using stemcells for Parkinsons.
Note:
Although there is a lot of excitement surrounding dopamine cell replacement therapy, we must proceed with care. The field has potential for setbacks from some of the less rigorous work being undertaken where regulatory standards are not as stringent as they perhaps should be or not meet the standards set by GForce-PD. These have the potential to halt proceedings on all cell replacement therapies.